

Article
CONFLICTED: Payer Pathways vs Their Own Coverage Policies
May 19, 2023Authors
Topics
Welcome to the May 2023 edition of our Monthly Insight Series. This month we are examining how Payers’ oncology pathways sometimes conflict with their own coverage policies, and how they can differ but still be aligned from a Payer perspective.

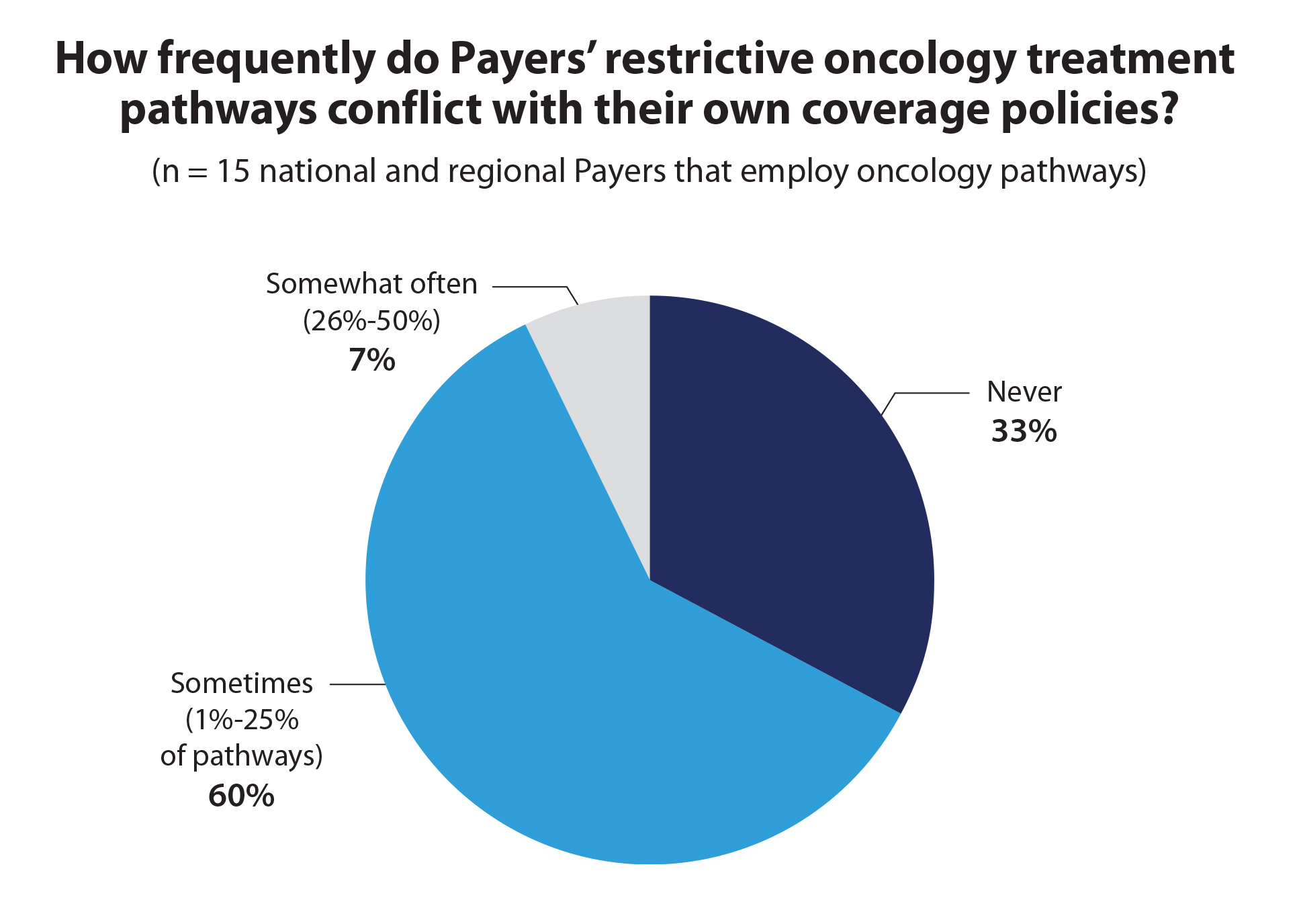
In 2022, half of our Payer survey participants said they use oncology pathways that restrict physician choice to 1-3 options with the intent to control costs and quality. Most of these Payers (67%) acknowledge that conflicts can (and do) exist between their pathways and their own coverage policies. An example of this is when a coverage policy restricts a patient from receiving a therapy that is “on pathway.”
Through numerous interviews, we’ve learned that pathway-policy “conflicts” are typically unintentional, and that Payers try to resolve them quickly.
It’s important to note, however, that our participating plans do not view pathways that simply restrict choice more than their associated drug coverage policies as conflicts:
- Payers view these policies and pathways as “aligned.”
- A Payer may attempt to circumvent Medicare coverage mandates through establishing a favorable coverage policy and then restrict choice of a brand through its pathway program.
- Payers may seek to enforce their pathways through the prior authorization process, denying an off-pathway selection and forcing either a changed prescription or a “peer-to-peer” discussion before potentially ultimately approving.
So then, we must also ask the questions: What is Payers’ real intent and what is the utility of payer pathways? Are they more analogous to speed limit signs, speed bumps, or traffic lights? HMP Market Access Insights plans to uncover this and much more later this year in our Payer report and in greater depth in our new pathway research program.
Have some “burning bridge” access questions of your own? Let us know!
All the best . . .
—HMP Market Access Insights Team: Chris, Cindy, Lee, Nandini, and Taylor
The Latest
Article
Notes From ATOPP: Providing Bispecific Antibody Treatments in Community Oncology
The ATOPP Summit covered a range of cutting-edge topics, including the shift toward administering cellular therapies to patients in community oncology settings.
Emma Bijesse, Daniel BuchenbergerArticle
Oncology Clinics Frustrated With Manufacturer Engagement Tactics
Welcome to the June 2024 edition of our Monthly Insight Series! This month we’re discussing oncology clinic concerns with existing manufacturer engagement approaches, using data drawn from our 2024 Community Oncology report, coming later in June.
Ashutosh ShethArticle
When Do Payer Pathways Matter?
While provider-initiated oncology clinical pathways are regaining momentum, payer pathways struggle to find a foothold in this space. Still, they can exert impact under certain conditions.
Cindy Chen





