

Article
Payer Insight: It’s NOT All About Drugs
October 16, 2023Authors
Topics
Welcome to the October 2023 edition of our Monthly Insight Series. This month we highlight a specific finding from our 2023 Payer Annual Oncology Trend Report that was just released in September: Payers’ top cancer cost targets.

Payers put drugs at center stage for cost control initiatives in oncology. This year’s report, however, illustrates that payers are also looking at other costs.
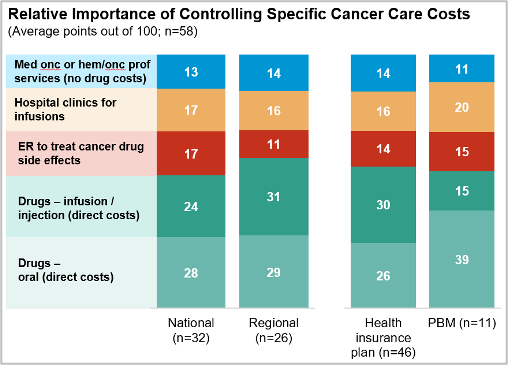
- Direct drug costs (orals and infusions/injectables combined) equate for ~half of Payers’ focus for controlling costs; nearly all Payers are also targeting other categories to some degree:
- Medical oncologist or hematologist/oncologist professional services (not including drug costs; 0-35 points across respondents; avg. 14 points)
- Infusions performed in hospital systems with high chargemaster reimbursement vs community infusion clinics or home infusion (0-60 points across respondents; avg. 16 points)
- Emergency room/department use for managing drug side effects (0-60 points across respondents; avg. 14 points)
- PBMs prioritize controlling costs of orals significantly more than infusions/injectables:
“Drug cost is our primary concern. We don’t try to control provider services costs, but we do have site-of-care programs.” – national vertical payer
A real-world example illustrates the factors that drive Payers’ drug cost focus in oncology:
An infused oncology product currently on the market costs ~$190,000/year. It is reported that ~20% of patients starting this therapy visit the ER/ED over the first 12 months of using it. The average cost for an ER visit for a patient with private insurance in 2019 was $2,453 (Kaiser, 2022). Using this ballpark average, even if the first-year ER/ED visits prompted by the infused oncology product were somehow prevented entirely, the savings would be arguably irrelevant: only 0.3% of the drug cost alone (ie, not including office visit costs for infusion/etc).
For further insights on the oncology sector, check out our other latest articles at https://www.hmpmarketaccessinsights.com/insights. From the Enhancing Oncology Model and integrated delivery network pharmacy performance metrics to payer pathways, we are sure to cover a topic that meets your needs!
The Latest
Article
IDN Financial Incentives: Impact on Treatment Prices?
Navigating IDNs requires understanding their financial drivers, revenue streams, and cost management. Here, we look at IDNs' key financial aspects, such as revenue optimization strategies, and examine the potential effects of site-neutral payment reforms.
Emma BijesseArticle
Provider Economics Drive Oncologist Consolidation
Welcome to the March 2024 edition of our Monthly Insight Series. This month we examine the trend of oncologists consolidating into IDNs and network aggregators.
Taylor CrutisonArticle
An Update on What You Need to Know About Pathways
Welcome to the February 2024 edition of our Monthly Insight Series, featuring key findings from our recent column in the Journal of Clinical Pathways. The column was the first in a series on oncologists' awareness and use of pathways.
Lee Blansett





